Abnormal heart rhythm / Atrial fibrillation
A change in the rhythm of your heart can cause it to beat either too quickly, or too slowly, or irregularly. This can affect your heart’s ability to pump enough blood to meet your body’s needs. If this is prolonged, it can result in heart failure.
Most abnormal heart rhythms can be treated with medicines. In more serious cases, you may require a medical device, radiofrequency ablation or surgery. If you have any concerns about your heart rhythm, you should discuss them with your doctor.
What is Atrial fibrillation?
Atrial fibrillation (AF) is the most common heart rhythm abnormality or cardiac arrhythmia. AF often coexists with heart failure. AF occurs when the upper chambers of the heart, also known as atria, have uncoordinated electrical activation and consequently ineffective atrial contraction. It is characterized by an irregular heart rate, which can be very rapid, and is diagnosed on an electrocardiogram (ECG).
These arrhythmia episodes can occur and then terminate spontaneously (called paroxysmal AF) or be continuous (called persistent or permanent AF). Factors contributing to the development of AF include advanced age, hypertension, diabetes mellitus, smoking, alcohol consumption, heart failure, coronary artery disease, chronic kidney disease, obesity and obstructive sleep apnea.
Consequences: Some patients clearly feel symptoms of AF while others may not feel them. Symptoms include palpitations, shortness of breath, fatigue, chest pain, poor exercise tolerance, dizziness, or more severe symptoms.
The two main risks of this common rhythm disturbance are: the development or deterioration of heart failure and stroke.
In AF, the atrial chambers have lost their contraction. This loss of the normal sequence of atrial and ventricular contraction may worsen pump function and increase heart failure symptoms. In addition, blood stagnation in the atria can lead to clot formation. In particular, the movement of these small clots in the general circulation can lead to stroke.
Management of the atrial fibrillation: Management of AF is tailored to the patient by a management team, adapted to each patient including a cardiologist, general practitioner and nurse. A psychologist, dietician, and pharmacist can all be part of the AF management team.
The treatment of this arrhythmia can be divided into 3 main areas:
-
- Anticoagulation therapy
Stroke risk and hemorrhage risk assessments are specific to each patient. Depending on these aspects, anticoagulation treatment (blood thinning) may be proposed. - Symptom control with control of the heart frequency or heart rhythm
Depending on each patient, many strategies can be proposed to control the heart rhythm.
These can for example be medications to slow down the heart, antiarrhythmic drugs, or treatments under anesthesia, e.g. blocking the arrhythmia using an electric shock to the heart or ablating it (marking its surface). - Management of cardiovascular risk factors:
Lifestyle modifications may be necessary, for example stop smoking, decrease alcohol consumption, modify diet and increase activity/exercise levels. The active involvement of each patient is an essential component in the successful management of AF.
- Anticoagulation therapy
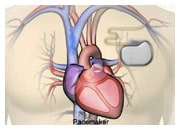
What does it do? Episodes of rapid heartbeat, either supra-ventricular from the upper chambers or ventricular arrhythmias from the main pumping chambers, are quite common and are frequently associated with a worsening of symptoms that may require hospitalisation. Medical therapy of heart failure decreases the frequency of such complications but often fails to eliminate them. When the risk of ventricular arrhythmias is high, an implantable cardiac defibrillator (ICD) can be implanted to treat these serious arrhythmias that can lead to worsening of symptoms or sudden death.
A catheter is a long thin tube or wire that can be inserted in a vein and moved up to the heart. Catheter ablation is currently the most efficient therapy to reduce arrhythmias or rhythm disturbances. In heart failure, changes within the cells of the heart may modify the pattern of electrical signals that make the heartbeat (electrical activation). Thus, some parts of the heart may activate spontaneously (premature contractions) or become part of an electrical loop or re-entry system that may lead to a persistent rapid heart rate. Catheter ablation aims to create superficial scars in the electrical conduction system of the heart to eliminate the area that triggers the arrhythmia, using a radiofrequency catheter or a cold application cryoballoon. Catheter ablation is often effective in eliminating or reducing the frequency of AF.
Catheter ablation is used for 2 main reasons:
- To decrease episodes of rapid heartbeat induced by supra-ventricular (atrial flutter, AF) or ventricular arrhythmias.
- To decrease the risk of sudden cardiac death (ventricular tachycardia, ventricular fibrillation).
Catheter ablation has been used for several decades and has been shown to reduce arrhythmias efficiently and to improve cardiac function in specific cases.
Catheter Ablation is made up of 3 parts:
- A diagnostic catheter to localize the electrical signals and map out the pattern of conduction.
- An ablation catheter to generate scar with different types of energy (radiofrequency, cryotherapy).
- A System to localize the position of the catheter in the heart (fluoroscopy or three-dimensional system).
How is it performed? Catheter introduction into the heart is performed by putting a tiny needle into vein, usually in the groin with local anesthesia. The first part of the procedure consists of studying and localizing the origin of the arrhythmia. Catheter ablation, which is often done in the same procedure, usually requires a light general anesthesia or sedation. Several applications of energy are performed to create small scars in the appropriate areas of the heart’s electrical conduction system. The success of the procedure is regularly tested to demonstrate that the abnormal electrical conduction cannot be triggered, and this defines the end of the procedure.
After the procedure: After the procedure, you will stay for 24-48 hours in a cardiology ward to monitor whether arrhythmia recurs. Depending on the arrhythmia and the procedure you may expect to be asked to rest slightly for a few days after going home.
Potentially rare, but possible, adverse events may include bleeding, a need for cardiac surgery, embolism (blood clot), arrhythmia, or injury to the electrical conduction system requiring you to have a pacemaker.
Recurrences of arrhythmia can occur within the first months due to some changes during the healing process. The procedure of catheter ablation can be performed several times to treat recurrence or other arrhythmias that may develop.