Pacemakers
What does it do?
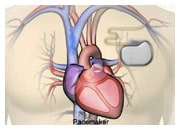
A pacemaker monitors your heart rate and sends small and painless electrical impulses to the right ventricle of your heart to start each heartbeat only when needed. You may need a pacemaker if your heart beats too slowly and it cannot be controlled by medication.
Pacemakers today are small metal devices, about the size of a small pocket watch, containing a computer and battery and up to three flexible electrode leads (coated wires). They are generally not visible, and apart from an insertion scar, which heals in time, they will usually become unnoticeable with time.
Where does it go and how is it put in place?
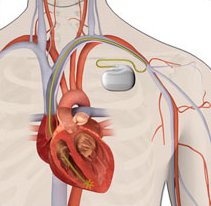
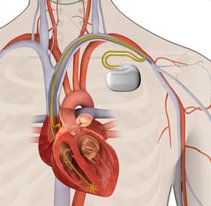
A pacemaker is usually implanted under local anaesthetic, just below your collarbone with leads (coated wires) coming from it that are positioned in your heart. The procedure usually takes 30-60 minutes.
The electrode lead is inserted into a vein at the shoulder or the base of the neck. The cardiologist guides the lead into the correct chamber of the heart, checking its position on an X-ray screen and securing it in position with a stitch at your shoulder. The lead is then connected to the pacemaker and the pacemaker is fitted into a small ‘pocket’, or space, between the skin and the chest muscle. The amount of electrical energy needed to stimulate the heart to contract is then tested and the pacemaker is adjusted.
After the procedure
After your pacemaker has been fitted, you may feel some pain or discomfort and there may be some bruising at the site of the pacemaker but these problems usually disappear in a few days. Most people are able to walk around later the same day and resume normal activities within a week.
The functioning and battery life of your pacemaker must be checked regularly at a pacemaker clinic. Depending on the device implanted, a telemonitoring follow-up may be proposed to monitor your pacemaker, allowing rapid identification of heart rhythm disturbance and technical dysfunction as well as improving your care and reducing the need for pacemaker clinic visits.
Only the device needs to be replaced (not the leads) if the battery runs out. The battery usually lasts between 6 and 10 years before it needs replacing.
It’s important that you let any doctors or dentists know that you have a pacemaker before going for any procedures. Although most medical and dental procedures are not likely to interfere with the functioning of your device, some may require precautionary measures that minimise any interference.
Pacemakers may sometimes be detected by airport security machines, so if you have a pacemaker you should always inform security personnel; however, the functioning of the device is rarely affected.
| There are two types of pacemakers |
 |
| Single-chamber pacemaker |
 |
| Dual-chamber pacemaker |