Left Ventricular Assist Devices (LVAD)
What does it do?
Some patients with advanced heart failure may not be suitable candidates for a heart transplantation. In addition, donor hearts are not always available and some patients may have to wait many years before a suitable donor heart is found. Mechanical circulatory support, or MCS, is a way to improve the circulation of blood throughout the body with a heart pump called a ventricular assist device (VAD). VADs will help your damaged heart to pump blood throughout the body. They are not a heart replacement and your heart will continue to function.
VADs will help to assist the normal function of the heart, prolong life and provide an improved quality of life for those with advanced heart failure. A VAD may be used for short-term support as a bridge-to-transplant (BTT), which means it can help a patient survive until a donor heart becomes available or used as destination therapy (DT), providing long-term support in patients who may be unsuitable for a heart transplant.
VADs are used for 3 main reasons:
- Keep patients alive until a donor heart can be found for transplantation. If this is the case, the VAD is used as a bridge-to-transplantation.
- Let the heart “rest” so that it can recover some of its normal function. In patients who have some heart recovery, the device can be removed and a heart transplant may not be needed at all. If this is the case, the VAD is used as a bridge-to-recovery.
- Support circulation over a period of years. This is usually the option for certain patients who are too sick to have a heart transplant. In this case, the VAD is used as destination therapy.
VADs have been approved for use in Europe for more than a decade. VAD therapy has improved survival and quality of life for advanced heart failure patients. Newer devices are smaller, quieter, and last longer. Patients have survived for several years with a VAD while waiting for a donor heart.
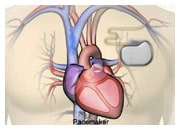
Almost all VADs are made up of 3 parts:
- A pump that is implanted inside the body (an implantable VAD) or placed outside the body (an external or paracorporeal VAD)
- A system controller that stays outside the body and is used to program the settings of the VAD
- An outside energy source to power the pump, either a console or a battery pack.
A VAD is a treatment option for certain patients with end-stage heart failure. Your doctor will determine if a VAD is an appropriate treatment for you.
Where does it go and how is it put in place?
Implanting a LVAD in a patient requires a surgical procedure under general anaesthesia. The cardiac surgeon will connect the device to the apex of the left ventricle and implant a cannula in the aorta to draw the blood from the ventricle and reinject it into the general circulation (left VAD) or the pulmonary artery (right VAD), increasing the blood flow in your body and improving the perfusion of your organs.
After the procedure
A few days in the post-operative care unit are often required, followed by a few days in a conventional ward to understand how to use the device. After that, a rehabilitation programme is often proposed to improve your exercise capacity. Potential adverse events may include: bleeding during surgery, infection, embolism and device malfunction. A VAD is designed to work for a long period of time. The device will alert you if there is a problem. The hospital will train you and your family to understand the device and its alarms.
Having a VAD will require some adjustments for you and your family. Managing the batteries is straightforward. Despite important technical progress, a percutaneous cable (driveline), connecting the internal pump to the external controller, is still necessary and the exit site dressing requires particular attention to prevent infection. Some heart failure medicines and anticoagulation therapy will need to be continued. However, most people who have a LVAD are able to live at home, move freely, enjoy their favourite activities, and even return to work or school. Many LVAD patients also find they have more energy than they did before, because more oxygen-rich blood is moving through their bodies. Please speak to your doctor or nurse at the hospital for more information.